Mpox (monkeypox)
Mpox (monkeypox)
EN ESPAÑOL: Mpox (viruela del mono)
Although the risk to most people is low, anyone can be affected by the human monkeypox (mpox). The virus spreads most commonly from prolonged, intimate skin to skin contact with an infected person’s rash or sores. For the most up to date data, visit the Centers for Disease Control and Prevention (CDC) and the Oregon Health Authority (OHA).
If you think you have been exposed to or have mpox, call a medical provider or Benton County Public Health at 541-766-6255.
On this page:
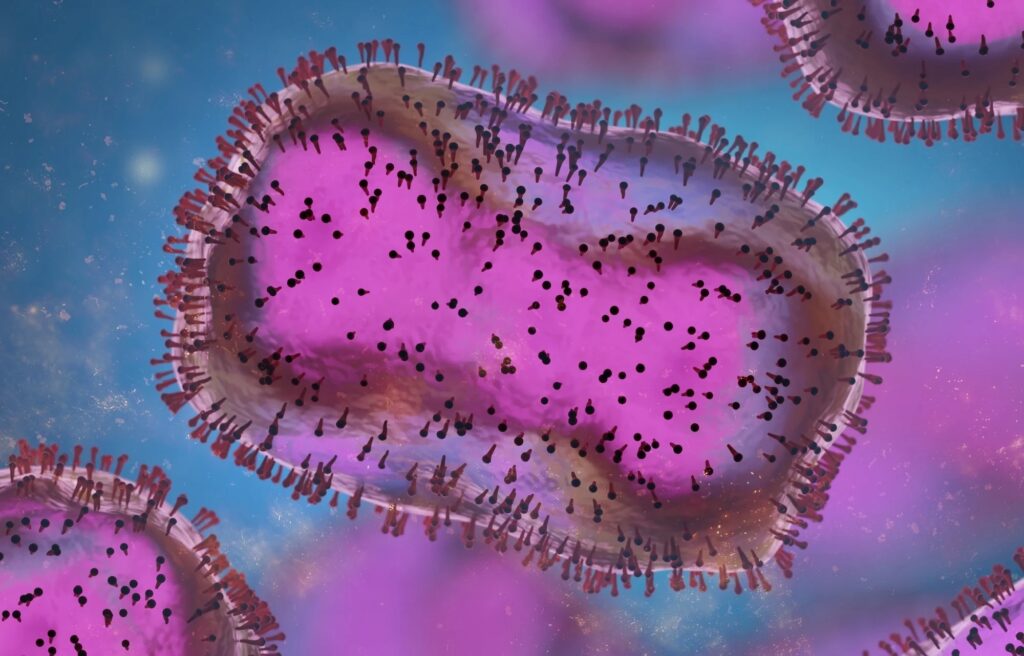
What is mpox?
Mpox is a virus that has caused small outbreaks in the USA over the last few decades. In relative terms, mpox does not spread like COVID-19, and is usually spread through skin to skin contact. Clinical studies continue to better understand mpox and how it spreads. The mpox virus is not limited to one community or another; anyone is susceptible to the virus.
Signs and Symptoms
The most common sign of mpox is a rash or sores (pox). The rash can look similar to acne, bug bites, or some sexually transmitted diseases. The rash may be hard to see. It can be painful or itchy and occur anywhere on the body including:
- Face
- Hands
- Chest
- Back
- Genital area
- Mouth
- Anus
- Rectum
The rash starts as raised bumps that then fill with fluid (clear to cloudy), turn into open sores, then scab over and disappear. This process usually takes 2-4 weeks.
Individuals may also have flu-like symptoms:
- Fever
- Swollen lymph nodes
- Chills
- Headache
- Muscle aches
- Fatigue
If you’re feeling sick and notice any new rashes – especially on the genitals or around the anus – avoid close skin-to-skin contact with others, and speak to a healthcare provider or call Benton County Public Health at 541-766-6255.
Spread or Transmission
In most cases, mpox is spread by:
- Close, prolonged skin-to-skin contact with someone who has mpox lesions. This is the most common method of infection and may include sex, cuddling, massage and kissing.
- Contact with towels, clothing or other objects that have been in contact with mpox lesions. Infection happens much less often this way.
- Respiratory droplets during extended face-to-face contact with someone who has mpox. This type of spread is uncommon.
Preventing Spread
Surveillance and rapid identification of new cases are critical for containing an outbreak. During mpox outbreaks, close contact with infected persons is the most significant risk factor for mpox infection.
- Avoid sex or other intimate contact if you or your partner have new skin wounds, fever, swollen lymph nodes or otherwise suspect exposure to mpox. Condoms do not prevent the spread of the virus (but do prevent the spread of other infections).
- Avoid contact with materials such as bedding that have been used for an extended period of time by someone infected.
- Wash hands thoroughly if you have contact with someone infected with mpox.
- If you develop symptoms, isolate yourself at home and contact a healthcare provider.
Vaccination
There is a vaccine that is safe and effective against mpox. Due to a limited supply, only certain people are eligible to receive it. The CDC recommends the vaccine be given within four days of exposure, if possible, to prevent onset of the disease. It can be given up to 14 days after exposure to reduce the symptoms.
If you think you may be eligible based on the current Oregon Health Authority criteria, please contact:
- Benton County Public Health at 541-766-6835, or
- Visit Samaritan Health Services’s scheduling portal
Testing and Treatment
Testing for mpox is available. Ask a health care provider about testing if you develop a new rash, bumps, or sores, especially if you know you have been in contact with anyone with the infection. If you do not have a health care provider, call Benton County Public Health, 541-766-6835.
Therapeutics have already been developed to treat similar illnesses which are effective against mpox, but are not widely available. Most people who become infected with mpox will recover without treatment. Treatment options can be discussed with a medical provider.
Community Partner Resources
For the most up to date data, community partner/organization guidance, and resources, visit the following links.
